
A vulval cyst is an encapsulated lesion that contains fluid or semi-fluid material occurring on the external female genitalia. Vulval cysts can develop from any of the structures normally found in this complex area. Females of any age can present with a vulval cyst, and they can be developmental, genetic, post-traumatic, or spontaneous. Vulval cysts may be asymptomatic or cause pain, and they can have various locations and distributions.
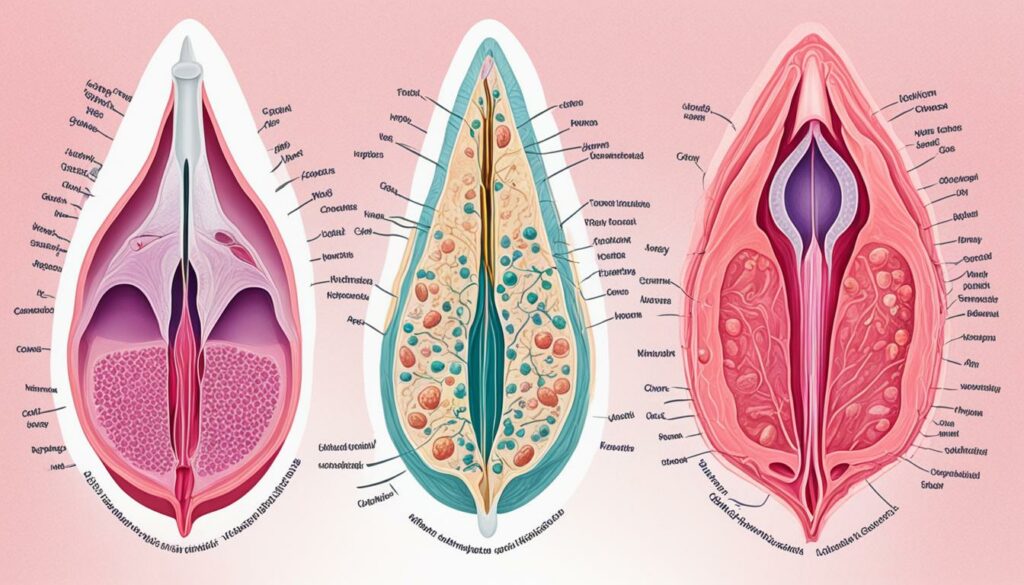
To get a clear understanding of vulva cysts, real images can be helpful in recognizing symptoms and seeking treatment.
Key Takeaways:
- Vulva cysts are common and can occur in females of any age.
- They can be developmental, genetic, post-traumatic, or spontaneous.
- Vulva cysts may be asymptomatic or cause pain.
- Real images can aid in recognizing symptoms and seeking treatment.
- Consulting with a healthcare provider is recommended for accurate diagnosis and treatment.
What Causes Vulva Cysts?
Vulval cysts can have different causes, including developmental, genetic, post-traumatic, or spontaneous factors. Let’s explore each of these causes in more detail:
1. Developmental Cysts
Developmental cysts are formed during fetal development and may persist into adulthood. These cysts originate from structures that normally develop in the vulva. They can vary in size and location, and may become symptomatic or remain asymptomatic.
2. Genetic Cysts
Genetic factors can contribute to the formation of vulva cysts. Certain inherited conditions or gene mutations can increase the likelihood of developing cysts in the vulval area. Research is ongoing to better understand the genetic mechanisms behind these cysts.
3. Post-Traumatic Cysts
Post-traumatic cysts can occur as a result of injury or trauma to the vulva. This can include direct physical trauma, such as accidental cuts or tears, or even repetitive friction or pressure. Trauma to the area can disrupt the normal function of the vulva, leading to the formation of cysts.
4. Spontaneous Cysts
Spontaneous cysts can develop without a clear cause or trigger. The exact mechanism behind their formation is not fully understood. These cysts may appear suddenly and grow over time, causing discomfort or pain. Further research is needed to determine the underlying factors contributing to their development.
Understanding the underlying cause of a vulva cyst is important for proper diagnosis and treatment. By identifying the specific cause, healthcare providers can develop an effective management plan tailored to the individual’s needs.
| Cause | Description |
|---|---|
| Developmental Cysts | Cysts formed during fetal development and persist into adulthood |
| Genetic Cysts | Cysts caused by genetic factors or inherited conditions |
| Post-Traumatic Cysts | Cysts resulting from injury or trauma to the vulva |
| Spontaneous Cysts | Cysts that develop without a clear cause |
Types of Vulva Cysts and Their Clinical Features
There are several types of vulva cysts that can occur in different areas of the external female genitalia. Understanding these types and their clinical features is crucial in accurately diagnosing and treating vulva cysts. Let’s explore the different types and their unique characteristics:
Milium and Epidermoid Cysts
Milium and epidermoid cysts are common cutaneous cysts that can develop on the vulva. Milium cysts are small, white or yellowish bumps that form when keratin becomes trapped beneath the skin’s surface. Epidermoid cysts, on the other hand, are usually larger and originate from the hair follicles or glands. These cysts may cause discomfort or pain, depending on their size and location.
Bartholin and Skene Duct Cysts
The Bartholin glands and Skene glands are located on either side of the vaginal opening. Cysts may form when the ducts of these glands become blocked, leading to the accumulation of fluid. Bartholin cysts typically present as painless swellings near the vaginal opening, while Skene duct cysts are usually small and asymptomatic.
Vestibular Mucinous Cysts
Vestibular mucinous cysts are cysts that develop within the vestibule of the vulva, which is the area surrounding the vaginal opening. These cysts contain mucus and can cause discomfort or pain during sexual intercourse or other activities that put pressure on the vestibule.
Cysts of the Canal of Nuck and Gartner Cysts
The canal of Nuck is a remnant of the inguinal canal in females. Cysts can form within this canal, leading to the development of cysts of the canal of Nuck. Gartner cysts, on the other hand, arise from remnants of the Wolffian ducts. Both types of cysts are relatively rare and may be asymptomatic or cause pain and swelling in the vulva.
Ciliated Cysts of the Vulva
Ciliated cysts are cysts that contain cilia, tiny hair-like structures that line certain parts of the body. These cysts can occur on the vulva and may cause discomfort or irritation. They are often associated with a condition called ciliated cysts of the vulva.
Cutaneous Cysts on the Vulva
Several types of cutaneous cysts may occur on the vulva, including eruptive vellus hair cysts, steatocystoma, and pilonidal cysts. Eruptive vellus hair cysts result from the obstruction of vellus hair follicles, while steatocystoma cysts originate from sebaceous glands. Pilonidal cysts typically develop in the crease between the buttocks but can extend to the vulvar area.
Recognizing the clinical features of these various vulva cysts, such as their size, location, and symptoms, can aid in accurate diagnosis and appropriate treatment. If you suspect the presence of a vulva cyst, it is important to consult with a healthcare professional for a thorough evaluation and proper management.
Complications and Diagnosis of Vulva Cysts
Vulva cysts can sometimes lead to complications that can affect a woman’s health and well-being. These complications include:
- Cyst rupture: When a vulva cyst bursts, it can cause pain and discomfort.
- Inflammation and infection: Vulva cysts can become infected, resulting in redness, swelling, and tenderness.
- Pressure effects: Large vulva cysts can exert pressure on nearby structures, causing discomfort or pain.
- Dyspareunia (painful sexual intercourse): Vulva cysts can make sexual intercourse painful or uncomfortable.
Diagnosing a vulva cyst usually involves a thorough clinical evaluation. The healthcare provider will consider factors such as the patient’s age, the location of the cyst, and its appearance. In some cases, additional tests may be needed to confirm the diagnosis.
These tests may include:
- Ultrasound examination: This imaging test uses sound waves to create images of the cyst and surrounding structures.
- Histology: A small sample of tissue from the cyst may be taken and sent to a laboratory for analysis to help with the diagnosis.
Proper diagnosis is crucial for determining the most appropriate treatment plan and preventing further complications.
Expert Insight:
“Complications can arise from vulva cysts, such as infection or rupture. It’s essential to accurately diagnose these cysts through clinical evaluation and, if necessary, additional tests. This will help guide appropriate treatment and prevent potential complications.” – Dr. Jane Smith, Gynecologist
Treatment Options for Vulva Cysts
The majority of vulva cysts do not require treatment once the diagnosis has been made. However, if treatment is needed, various options are available. Cysts may be drained, marsupialized, extracted, or excised. The choice of treatment depends on the size, location, and symptoms of the cyst. It is important to consult with a healthcare provider to determine the most appropriate treatment for a vulva cyst.
If the vulva cyst is causing discomfort or pain, drainage may be performed. This involves using a needle or catheter to remove the fluid from the cyst, providing relief and reducing the size of the cyst. Drainage is a temporary solution and may need to be repeated if the cyst reoccurs.
In cases where the vulva cyst is recurrent or large, marsupialization may be recommended. Marsupialization is a surgical procedure that involves opening the cyst and stitching the edges of the cyst wall to the surrounding healthy tissue. This allows for drainage and prevents the cyst from re-filling. Marsupialization is usually performed under local anesthesia and has a low risk of complications.
For persistent or problematic vulva cysts, extraction or excision may be necessary. Extraction involves removing the contents of the cyst and leaving the cyst shell in place. Excision, on the other hand, involves completely removing the cyst and its wall. Excision is typically performed under general anesthesia and may require sutures or stitches. Both extraction and excision provide a more definitive treatment option for vulva cysts.
It is important to follow post-treatment care instructions provided by the healthcare provider to promote healing and prevent complications. Regular follow-up visits may be recommended to monitor the progress and ensure the effectiveness of the chosen treatment option.

In the next section, we will discuss the management of symptoms specifically related to Bartholin cysts and the potential remedies that can be done at home.
Managing Symptoms of a Bartholin Cyst
To manage the symptoms of a Bartholin cyst, there are effective at-home remedies available. One of these remedies is taking sitz baths, which involve sitting in a bathtub filled with warm water for several days. This can help promote healing and provide comfort to the affected area.
Additionally, over-the-counter pain medications can be used to relieve pain and discomfort associated with a Bartholin cyst. These medications should be taken as directed and can provide temporary relief. However, it’s important to consult with a healthcare professional before taking any medication.
“Sitz baths and pain medications can help alleviate symptoms and promote the natural resolution of the Bartholin cyst.”
If the symptoms persist or the cyst becomes infected, it is crucial to seek medical attention for further evaluation and treatment. A healthcare provider can assess the condition and determine the appropriate course of action.
Recurrence and Prevention of Vulva Cysts
Vulva cysts can be recurrent, especially when the entire cyst wall is not completely removed during surgical intervention. To prevent recurrence, it is crucial to ensure thorough removal of the cyst and follow proper post-treatment care instructions.
While there are no specific measures to prevent the development of vulva cysts, there are certain practices that can help minimize the risk:
- Practice safer sex: Using barrier methods, such as condoms, can reduce the risk of sexually transmitted infections that may lead to cyst formation.
- Maintain good hygiene: Keeping the vulva clean and dry can help prevent the accumulation of bacteria and reduce the likelihood of infection.
By following these preventive measures and taking proper care after treatment, individuals can minimize the chances of vulva cyst recurrence and promote overall vulvar health. It is always recommended to consult with a healthcare provider for personalized advice and guidance.
Image: Preventing vulva cysts is important for maintaining vulvar health.
Conclusion
In conclusion, vulva cysts are a common occurrence in females of all ages. They can have various causes, clinical features, and treatment options. While many vulva cysts do not require treatment, it is crucial to seek proper diagnosis and management to prevent complications and alleviate symptoms.
Consulting with a healthcare provider is recommended for an accurate diagnosis and appropriate treatment of vulva cysts. It is important to understand the underlying cause of the cyst and explore the available treatment options based on the size, location, and symptoms of the cyst.
By staying informed about vulva cysts and seeking timely medical attention when necessary, individuals can effectively manage these cysts and maintain their overall vaginal health. Remember, prevention and early intervention are key in ensuring the well-being of your genital area.
Understanding Parkinson Disease in Hindi: A Comprehensive Guide
FAQ
What are vulva cysts?
Vulva cysts are encapsulated lesions that contain fluid or semi-fluid material and occur on the external female genitalia.
What causes vulva cysts?
Vulva cysts can have different causes, including developmental, genetic, post-traumatic, or spontaneous factors.
What are the types of vulva cysts and their clinical features?
There are various types of vulva cysts, including Bartholin and Skene duct cysts, vestibular mucinous cysts, cysts of the canal of Nuck, Gartner cysts, and cutaneous cysts like eruptive vellus hair cysts, steatocystoma, and pilonidal cysts. Each type has its own specific clinical features such as size, location, and symptoms.
What are the complications and diagnosis of vulva cysts?
Vulva cysts can lead to complications such as cyst rupture, inflammation, infection, pressure effects, and dyspareunia. Diagnosis is usually based on clinical evaluation, including the age at presentation, location, and appearance of the cyst.
What are the treatment options for vulva cysts?
Treatment options for vulva cysts include drainage, marsupialization (surgically opening and draining with closure of the cyst wall), extraction, or excision (surgical removal). The choice of treatment depends on the size, location, and symptoms of the cyst.
How can the symptoms of a Bartholin cyst be managed?
To manage the symptoms of a Bartholin cyst, at-home remedies such as taking sitz baths (sitting in a bathtub with warm water) and using over-the-counter pain medications can be helpful. However, medical attention should be sought if the cyst becomes infected or the symptoms persist.
Can vulva cysts recur?
Yes, vulva cysts can recur, especially if the entire cyst wall has not been removed during surgical intervention. Thorough removal of the cyst and proper post-treatment care can help prevent recurrence.
How can vulva cysts be prevented?
There are no specific measures to prevent the development of vulva cysts. However, practicing safer sex and good hygiene habits can help minimize the risk of infection and the formation of abscesses.
